Thrombosis complication in Post Fontan Surgery
Category: Peripheral, Congenital, Complication,
Introduction
Thromboembolism is a complication that may happen in Fontan surgery, despite therapeutic international normalized ratio (INR). There are few studies in the literature to determine the epidemiology of thrombosis after Fontan. The incidence of thrombosis has not been determined by prospective trials despite that some cross sectional surveys using transesophageal echocardiography found that the prevalence of thromboembolism following Fontan surgery ranges between 17% and 33%. This can occur both early and late after the procedure with the highest during the first year.
History
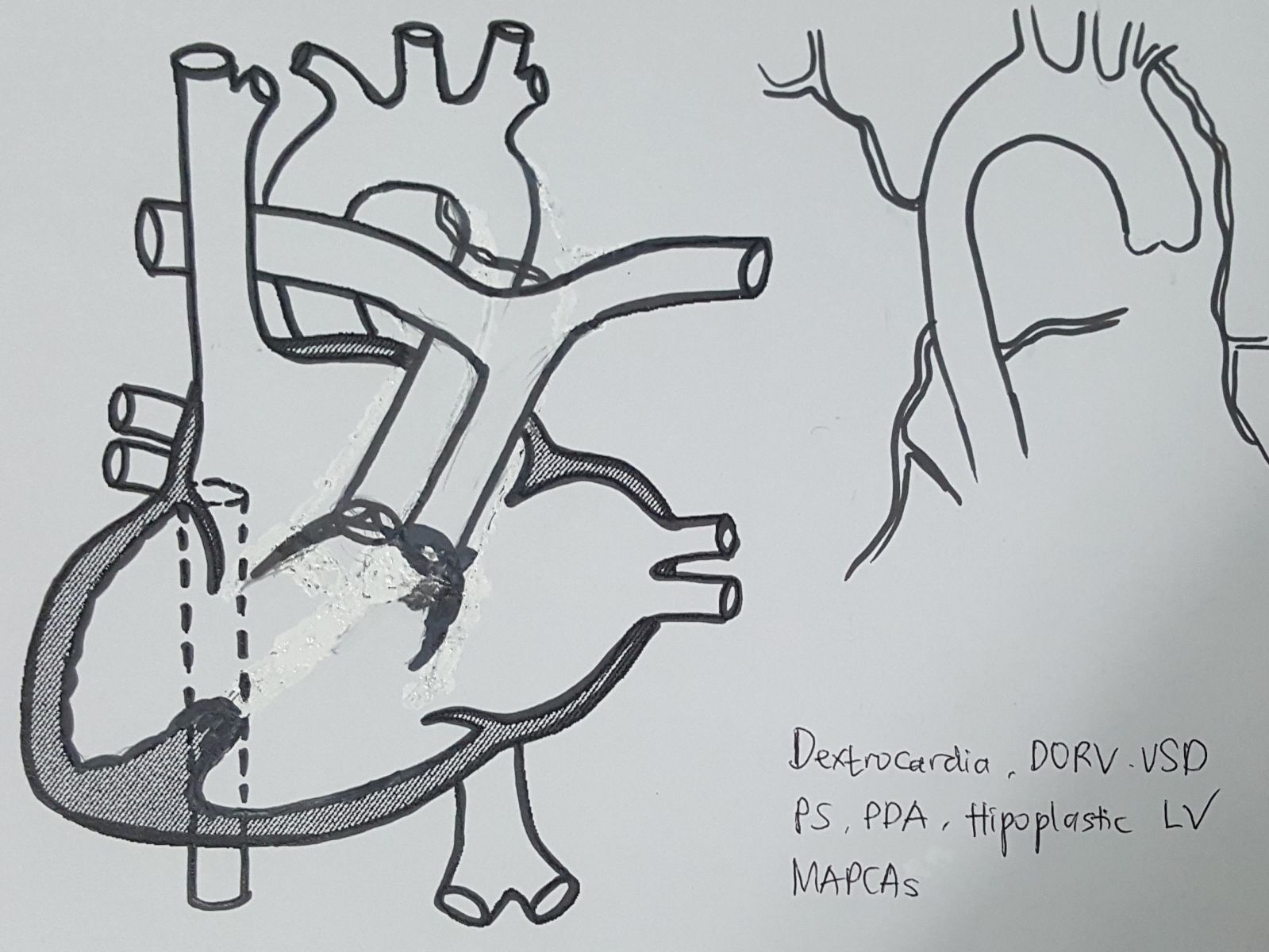
An 11-year-old girl who firstly came to our center (PJNHK) at age 7 with chief complaint of bluish, and was diagnosed as Dextrocardia, situs solitus, double outlet right ventricle (DORV), hypolastic left ventricular (LV), inlet muscular type of ventricular septal defect (VSD), severe pulmonary stenosis (PS), patent ductus arteriosus (PDA) and major aorto-pulmonary colateral arteries (MAPCAs). Patient was planned for a ventricular one-way repair operation, and an initial stage of Bluntock-Taussig (BT) shunt surgery was performed to enlarge the diameter of the pulmonary artery. Two years later bidirectional cavo-pulmonary shunt (BCPS), atrial septectomy, left pulmonary artery (LPA) repair, PDA and BT shunt ligation were done followed by MAPCAs embolization at the following year. A month afterward, Fontan surgery was done with good result.

Findings
On the 8th day postoperative, a long, large (10x14mm) thrombus in the inferior caval vein (IVC) was found on echocardiography although she was still in intravenous anticoagulant therapy (Figure 1). Anastomosis of IVC to extra-cardiac conduit and superior caval vein (SVC) to right pulmonary artery (RPA) is good. Then we decided to continue the anticoagulant for 3 days, but thrombus still found with relatively similar size. Patient was without complaints, no abnormalities found on physical examination and blood coagulability.
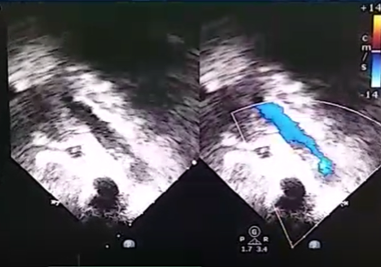
Figure 1. Thrombus in IVC from TTE
Procedure
Almost all cases of thrombosis in Fontan can be treated with anticoagulation without the need for intervention. But in this case the management with intravenous anticoagulation is unsuccessful. From discussions with the team, it was decided to carry out thrombus aspirations and thrombolysis directly through the catheter. Procedure was performed via right femoral vein with 10F sheath. The 8F guiding catheter was inserted through the sheath and slowly pushed into the iliac vein and IVC while aspiration of the thrombus was simultaneously performed. An angiographic evaluation showed no blood flow through the femoral vein and the contrast did not fill IVC due to thrombus (figure 2).

Figure 2. The thrombus totally blocked the lumen of IVC to proximal right iliac vein
Thrombus aspiration was repeated many times and the catheter pushed up to the IVC (figure 3). Unfortunately, the thrombus was actively produced and indestructible. Then we decided to stop and proceded to do directly thrombolysis with r-TPA through a catheter in IVC.

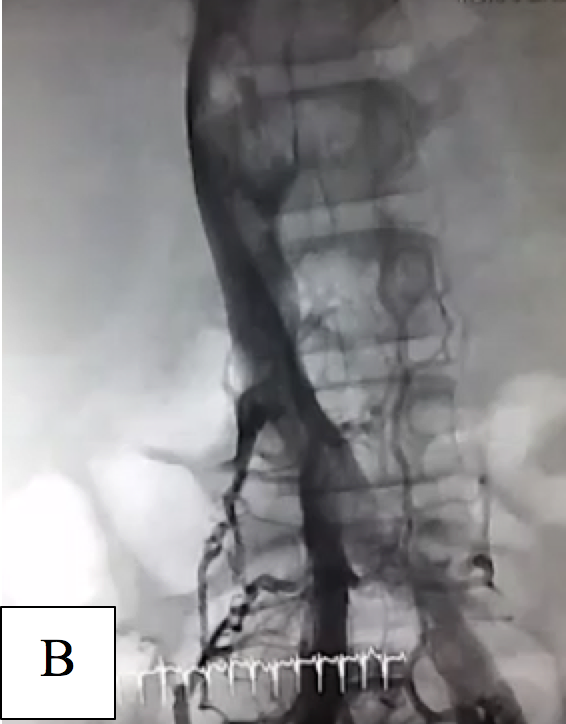
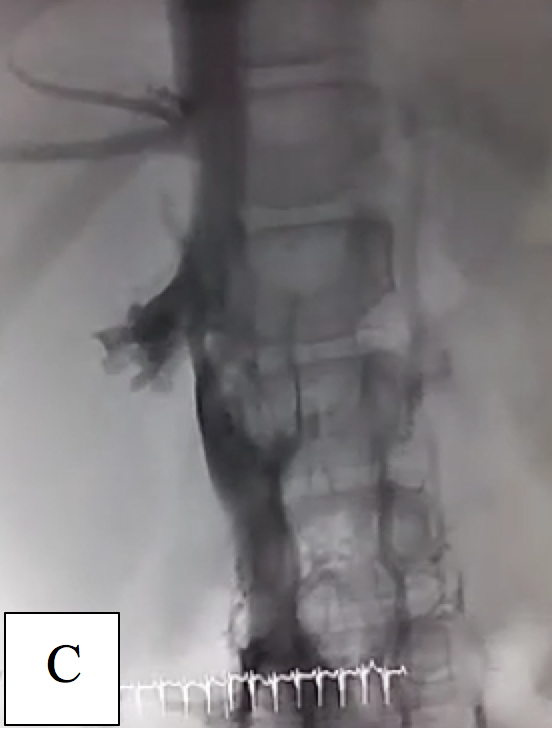
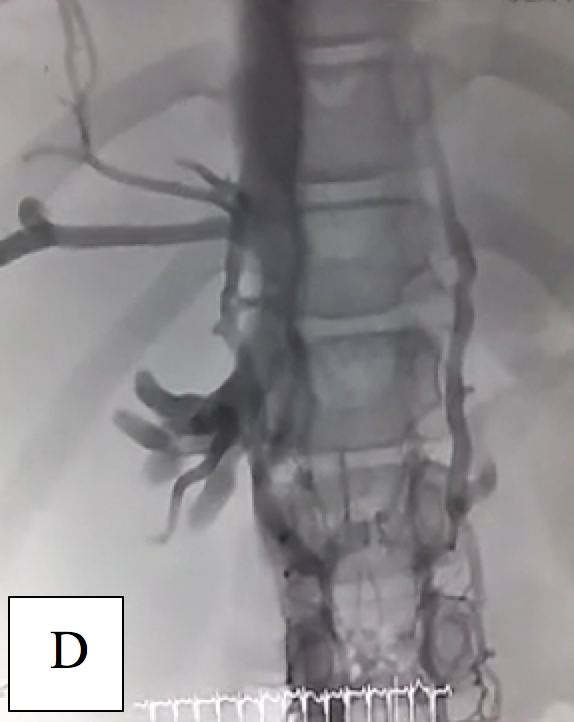
Figure 3. The flow was seen after recurrent thrombus aspiration. (A) limited flow in right iliac vein, (B) the contrast began to fulfil the iliac vein, (C) and (D). flow was clearly visualized filling the IVC, residual thrombus was detected.
The catheter was modified by making numerous holes along the proximal portion of the catheter with a distance of ± 1cm, then placed in IVC. r-TPA was inserted with a dose of 2 mg bolus followed by 1.5mg / hour. Peripheral intravenous of heparine was also given 5 units / kgBW / hour. Thrombolysis procedure were planned for 24 hours and periodic evaluations of general conditions, thrombus sizes and blood fibrinogen values were performed every 4 hours. r-TPA would be discontinued when the fibrinogen value <100 mg/dL or bleeding occured. After 10 hours, r-TPA was stopped due to low level of fibrinogen (40mg/dL) and thrombus size decreased. Intravenous heparine was continued for up to 8 days, and overlapped with oral anticoagulants (warfarin). The patient was eventually discharged in good condition. Echocardiography evaluation 1 week and 3 months later, showed no thrombus in the IVC nor in the extra-cardiac conduit.
.png)
.png)
Figure 4. Echocardiography evaluation after thrombolysis
Discussion
Thromboembolism in post-operative Fontan patients are primarily due to the slow flow of IVC to the pumpless of RV to pulmonary circulation, impaired blood coagulability, arrhythmias and Fontan circulatory tract obstruction. Regularly and chronically use of oral anticoagulants may not prevent thrombosis. Prompt and appropriate intervention is needed to prevent pulmonary embolism and total IVC blockage that can lead to death. This complication can be managed with surgical thrombectomy, thrombus aspiration, intravenous thrombolysis, and stent insertion intervention in the case of Fontan circulatory stenosis. Directed catheter thrombolytic particularly for IVC thrombosis in postoperative Fontan is almost never reported. However, general use in extensive thrombosis and proximal veins (IVC) is one of the major indication. To date, surgical thrombectomy has become the first choice of thrombus management in NCCHK. Nonetheless, after this case, other modalities with lower risk can be considered. Directed catheter thrombolytic has been proved to be effective and can maintain the patency of the Fontan circulation which will decrease morbidity and mortality. The use of recombinant tissue type plasminogin activator (r-TPA) has been shown to be safe and effective and significantly indicates better clinical outcomes in both short and long-term follow-up.
References:
Monagle P, Cochrane A, Roberts R, et al. A multicenter, randomized trial comparing heparin / warfarin and acetylsalicylic acid as primary thromboprophylaxis for 2 years after the Fontan procedure in children. J Am Coll Cardiol. 2011;58(6):645-51.
David NR, Alan HF, Charles SK, Gary SK, Lynda ER, William EH. Thromboembolic complications after Fontan operations. Circulation 1995;92:287-93.
Raja N, Agarwal S, Tomar AS, Geelani MA, Srivastava S. Complete Thrombosis of the Conduit and Inferior Vena-cava Early After Extracardiac Fontan Operation. MAMC J Med Sci 2017;3:28-30.
Al-Biltagi M, Al-Kouatli A , Al-Ata J, Jamjoom A., Abouzeid H. Thrombosis of Extra-cardiac Fontan, an Institutional Experience. Cardiology and Angiology: An International Journal 2015;3(4): 192-202.,
BC Srinivas BC, Singh AP. Successful Thrombolysis of Occluded Inferior Vena Cava Filter with IVC Syndrome. J Cardiovasc Thorac Res. 2012; 4(4): 119–122.
Golowa Y, Warhit M, Matsunaga F, and Cynamon J. Catheter directed interventions for inferior vena cava thrombosis. Cardiovasc Diagn Ther. 2016 Dec; 6(6): 612–622.
Gomaa M, Fahmy H, Farouk A. Catheter direct thrombolysis: Role of actilyse in treatment of acute deep venous thrombosis. The Egyptian Journal of Radiology and Nuclear Medicine2013;44: 57-62.
Augustinas P, Ouriel K. Invasive approaches to treatment of venous thromboembolism. Circulation 2004;110:1-34.

